
Glucose is a type of sugar. It comes from food and also is created in the liver. Glucose travels through the body in the blood. It moves from the blood to cells with the help of a hormone called insulin. Once glucose is in those cells, it can be used for energy. Diabetes mellitus is a condition that causes a buildup of glucose in the blood and makes it difficult for the body’s cells to get enough energy. There are two primary kinds of diabetes mellitus, type 1 and type 2.
In short, both types result in high levels of blood glucose. Type 1 is an autoimmune disease, caused by genetic and environmental factors, that results in too little insulin being produced by the body. Type 2 is influenced by lifestyle choices and results in the body not being able to use its insulin efficiently. According the Centers for Disease Control (CDC), “Type 2 diabetes accounts for about 90% to 95% of all diagnosed cases of diabetes, and type 1 diabetes accounts for about 5%.”
Overview of Type 1 and Type 2 Diabetes
Type 1—An autoimmune disease occurs when there is an abnormal immune response to a normal part of the body. Type 1 diabetes is an autoimmune disorder caused by destruction of the cells that secrete insulin from the pancreas. This results in too little insulin being produced to support the body’s needs. Type 1 diabetes is usually diagnosed in children and young adults, and was previously known as juvenile diabetes.
Without insulin, glucose from the carbohydrate foods you eat cannot enter cells. This causes glucose to build up in the blood, leaving your body’s cells and tissues starved for energy. While a variety of tissue transplantation and genetically-based treatments are being studied, at this point the only widely-available treatments for type 1 diabetes are the injection of insulin and inhaled insulin.
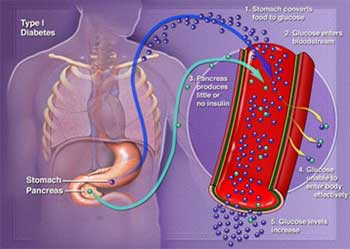
Copyright © Nucleus Medical Media, Inc.
Image text:
- Stomach converts food to glucose
- Glucose enters the bloodstream
- Pancreas produces little or no insulin
- Glucose unable to enter body effectively
- Glucose increases
Type 2—Type 2 is the most common form of diabetes and can be caused by a combination of factors. One factor is that your body begins to make less insulin. A second is that your body becomes resistant to insulin. This means there is insulin in your body, but your body cannot use it effectively. Insulin resistance is often related to excess body fat. Medication, lifestyle changes, and monitoring can help control blood glucose levels in those with type 2 diabetes.
Symptoms
Type 1—Symptoms of type 1 diabetes are caused by the buildup of glucose in the blood and the lack of glucose in body cells, known as hyperglycemia. Symptoms include:
- Unexplained weight loss
- Increased urination
- Extreme thirst
- Hunger
- Fatigue, weakness
- Blurry vision
- Irritability
- Headaches
- Nausea, diarrhea, or constipation
- Chest pain
- Confusion
- Coma
Type 2—You may have type 2 diabetes for years before you have symptoms:
- Increased urination
- Extreme thirst
- Hunger
- Fatigue
- Blurry vision
- Irritability
- Frequent or recurring infections
- Poor wound healing
- Numbness or tingling in the hands or feet
- Problems with gums
- Itching
- Problems having an erection
Risk Factors
Type 1—Risk factors for developing type 1 diabetes include:
- Family History of type 1 diabetes
- Other autoimmune conditions such as Hashimoto disease, Graves’s disease, lupus, and rheumatoid arthritis.
- Certain ethnic groups such as Northern European, Mediterranean, African American, Hispanic, or Native American
- Other risk factors that may influence getting type 1 diabetes are:
- Cystic fibrosis
- Bottle feeding or a short duration of breast feeding
- High birth weight
- Childhood obesity
- If a mother’s age at child birth was over 35 years
Type 2—Risk factors for developing type 2 diabetes include:
- Being over the age of 45
- Prediabetes—impaired glucose tolerance and impaired fasting glucose
- Metabolic syndrome—a condition marked by elevated cholesterol, blood glucose, blood pressure, and central obesity
- Excess weight or obesity
- Lack of exercise
- Poor diet—high intake of processed meats, fats, and sugar-sweetened foods and beverages
- Family history of type 2 diabetes
- High blood pressure
- History of cardiovascular disease
- Depression
- History of gestational diabetes, or having a baby that weighs over 9 pounds at birth
- Endocrine disorders, such as Cushing’s syndrome, hyperthyroidism, acromegaly, polycystic ovary syndrome, or acute pancreatitis
- Certain medications, such as glucocorticoids or thiazides
- Certain ethnic groups, such as African American, Hispanic, Native American, Hispanic American, Asian American, or Pacific Islander
Treatment
Type 1—Type 1 diabetes is a chronic disease that has no cure, but it can be managed with proper treatment and care. The goal of diabetes treatment is to maintain blood glucose levels before and after meals within a healthy range. By doing so, you will feel better on a daily basis and will help prevent or delay complications of diabetes. Talk to your doctor about what a healthy blood glucose range is for you.
The main components of treatment are:
- Insulin
- Blood glucose monitoring
- Diet
- Exercise
- Glucagon for emergency management of hypoglycemia
Type 2—Treatment aims to maintain blood sugar at levels close to normal, prevent or delay complications, and control other conditions that you may have, like high blood pressure and high cholesterol. Treatments include:
- Diet—Food and drinks have a direct effect on your blood glucose level. Eating healthy meals can control your blood glucose. It will also help your overall health. Some basic tips include:
- Follow a balanced meal plan that includes carbohydrates, proteins, and fats.
- Eat normal serving sizes. Measure your food control portion sizes, if necessary.
- Do not skip meals. Having meals throughout the day can maintain steady glucose levels.
- Eat plenty of vegetables and fiber.
- Limit the amount of fat, especially saturated and trans fats, in your foods.
- Eat moderate amounts of protein and low-fat dairy products.
- Carefully limit foods containing high concentrated sugar.
- Keep a record of your food intake and create a meal plan with your dietician or doctor.
- Weight Loss—If you are overweight, weight loss will help your body use insulin better. Talk to your doctor about a healthy weight goal. These options may help you lose weight:
- Use a portion control plate
- Use a prepared meal plan
- Eat a Mediterranean-style diet
- Exercise— Physical activity can:
- Make the body more sensitive to insulin
- Help you reach and maintain a healthy weight
- Lower the levels of fat in your blood
- Aerobic exercise increases your heart rate and resistance training build muscle strength. Both types of exercise help to improve long-term glucose control
- Medication—Certain medications will help to manage blood glucose levels. Talk to your doctor about special medication to help control your diabetes.
- Insulin— Insulin usually is given through injections and may be needed if:
- The body does not make enough of its own insulin
- Blood glucose levels cannot be controlled with lifestyle changes and medications
- Blood Glucose Testing—You can check the level of glucose in your blood with a blood glucose meter. Checking your blood glucose levels during the day can help you stay on track. It will also help your doctor determine if your treatment is working. Keeping track of blood sugar levels is especially important if you take insulin.
More information can be found on the American Diabetes Association website- www.diabetes.org. For individual diagnosis and treatment recommendations for type 1 and type 2 diabetes, please consult your physician. Joyce Vivian, MSN, NP, is available to screening, treatment options, and lifestyle tips. To schedule an appointment, call the office at (540) 772-3490 or schedule an appointment online.
Book An Appointment Online with Joyce Vivian, MSN, NP
Sources:
Centers for Disease Control (CDC): www.cdc.gov
CDC - Diabetes (PDF)
American Diabetes Association: diabetes.org