
A Whipple procedure, also known as pancreaticoduodenectomy, is the primary surgical treatment for pancreatic head cancer. It is named for the American surgeon Allen Whipple, who refined the technique that was used in earlier surgeries. According to the American Cancer Society, a Whipple procedure is a complex operation that “removes the head of the pancreas and sometimes the body of the pancreas, as well. Nearby structures such as part of the small intestine, part of the bile duct, the gallbladder, lymph nodes near the pancreas, and sometimes part of the stomach are also removed.”
The Pancreas
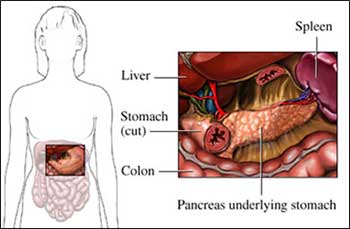
Copyright© Nucleus Medical Media, Inc.
Reasons for the Whipple Procedure
You may have this surgery to treat cancer of the pancreas, duodenum, or lower part of the bile duct. It also may be done to treat people with chronic pancreatitis.
What to Expect Before, During, and After the Procedure
Prior to the Procedure
Before the surgery, your doctor may do the following tests:
- Physical exam.
- Blood tests.
- Echocardiogram (EKG) to check your heart function.
- Lung function tests to make sure your lungs are strong.
- Imaging tests to locate the cancer and make sure it has not spread.
Your doctor may put you on a special diet before the surgery to help your body prepare. If you are not able to eat, you may need to go to the hospital several days before surgery. You will be given glucose and fluids through an IV. Talk to your doctor about your medications, herbs, and dietary supplements. You may be asked to stop taking some medications up to one week before the procedure.
Before your procedure, talk to your doctor about ways to manage factors that may increase your risk of complications, such as:
- Smoking.
- Drinking.
- Chronic diseases, such as diabetes or obesity.
Anesthesia
General anesthesia will be used. It will block any pain and keep you asleep during surgery.
Description of the Procedure
For open Whipple procedures, a large incision will be made in the abdomen. The head of the pancreas and the gallbladder, duodenum, and pylorus will be removed. Nearby lymph nodes may also be removed. The remaining pancreas and digestive organs will be reconnected. This will allow the digestive enzymes from the pancreas and stomach contents to flow into the small intestine. In some cases, the pylorus is not removed. The doctor will close the incision with stitches or staples. The incisions will be covered with bandages.
For laparoscopic procedures, a camera and small surgical instruments are inserted through small incisions into the abdomen. The organs can be removed and reconnected through the openings. After the area is carefully examined, the laparoscope will be removed. The doctor will close the incision with stitches or staples. The incisions will be covered with bandages.
You may have many small tubes placed after the procedure. Some will help drain fluid from the surgery site. Another tube may go into your stomach to help prevent nausea and vomiting. A tube may go to your intestines so you can receive nutrition.
Whipple Procedure
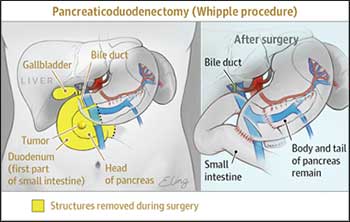
Source: JAMA Network®
Immediately After the Procedure
After surgery, you will stay in the intensive care unit for several days. This will help the doctors and nurses monitor your progress.
How Long Will It Take?
4-8 hours
How Much Will It Hurt?
Anesthesia will prevent pain during surgery. Pain and discomfort after the procedure can be managed with medications.
Average Hospital Stay
You will need to stay in the hospital until your intestines begin to work again. This usually takes 2 weeks. You may need to stay longer if there are any problems.
Post-procedure Care
At the Hospital:
During surgery, your doctor may have placed a jejunostomy tube (j-tube). You will receive nutrients through this tube until your intestines are working normally. After the tube is removed, you can gradually progress to a soft diet, then to regular food. Other tubes will be removed as you recover.
Preventing Infection:
During your stay, the hospital staff will take steps to reduce your chance of infection, such as:
- Washing their hands.
- Wearing gloves or masks.
- Keeping your incisions covered.
There are also steps you can take to reduce your chance of infection, such as:
- Washing your hands often and reminding your healthcare providers to do the same.
- Reminding your healthcare providers to wear gloves or masks.
- Not allowing others to touch your incision.
At Home
This surgery will affect the way your body digests food. You may feel bloated or full after eating. You may have nausea and vomiting. Talk to your doctor or dietitian to learn how you should eat. You may need to start new medications to help with digestion and medications to help control your blood sugar. Follow instructions about wound care to prevent infection.
When to Contact Your Doctor
Contact your doctor if your recovery is not progressing as expected or you develop complications, such as:
- Signs of infection, such as fever or chills.
- Redness, swelling, increasing pain, bleeding, or discharge from the incision.
- Pain that is not controlled with the medications you were given.
- New or worsening:
- Diarrhea
- Weigh loss
- Nausea and/or vomiting
- Symptoms of diabetes, which may include:
- Frequent urination
- Excessive thirst
- Increased hunger
- Slow wound healing
If you think you have an emergency, call for medical help right away.
Potential Complications
Even under the best circumstances, patients may have complications from Whipple procedure surgery. These can include:
- Trouble with the stomach emptying after eating (gastroparesis).
- Trouble digesting some foods (which might require taking pancreatic enzyme supplements).
- Leaking from connections made in the intestines.
- Chronic abdominal pain.
- Damage to other organs.
- Bleeding.
- Infection.
- Reaction to anesthesia.
- Blood clots.
- Weight loss.
- Changes in bowel habits.
- Diabetes.
Sources:
American Cancer Society:cancer.org
American Cancer Society: Surgery for Pancreatic Cancer
Journal of American Medical Association: Pancreatic Operations: jamanetwork.com
If you suspect you have symptoms of pancreatic head cancer, please consult your healthcare provider immediately. Dr. Dominique Dempah of LewisGale Physicians can answer all of your questions and discuss surgical options. To schedule an appointment, call the practice at (540) 772-3620 or book an appointment online below.
Book An Appointment Online with Dr. Dominique Dempah